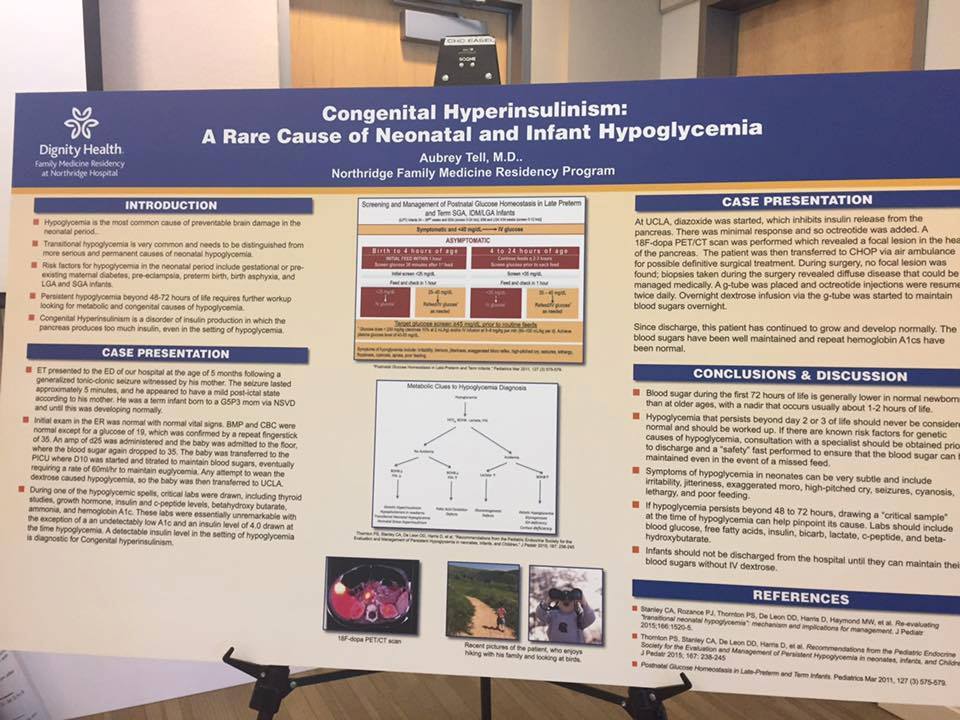
Combining her personal experience with medical knowledge, Aubrey Tell, HI mom and family practice doctor, has created a presentation about HI for medical residents:
“I think the most important thing we can do is educate people that HI exists, and if there are any symptoms of hypoglycemia in a neonate, even if they don’t have any risk factors, we should have a very low threshold for checking a blood sugar. I would love to see more research in this area as well as to the best way to make sure these cases are not missed going forward.”
In this interview, Aubrey discusses her son Ezra’s hyperinsulinism journey, and provides thoughtful input on the importance of personal HI stories for medical professionals, complications of testing for HI in newborns.
Tell us a little bit about yourself, your son, and your experience living with HI:
I am Aubrey, married to Jeff for 13 years, and the mother of three children: Judah, Naomi, and Ezra. I’m also a family practice doctor who works part time in Northridge, California. Ezra was born December 1, 2014, weighing 6 pounds, 12 ounces. It was an easy labor and delivery and he seemed totally normal. For the first five months, everything was great. He was a great eater, a great sleeper, and a perfect, happy baby. Then, at the age of 5 months, I was at the grocery store, carrying him in an erg, while I shopped, and he suddenly had a seizure. It lasted 5 terrifying minutes. I called 911 but by the time I got through, the seizure had stopped so I quickly put him in the car and drove to the hospital where I work. At the ER, we were seen fairly quickly and labs were drawn, although Ezra seemed to be back to his normal self. Just a short time later, his blood sugar came back at 19. I had never actually seen a blood sugar that low. The nurse thought it was an error and rechecked a fingerstick which was also very low. He was admitted and given fluids to bring his blood sugar back up. Once we got to the floor, his blood sugar dropped again into the 30s and so we were transferred to the ICU and started on a high rate of fluids to try to maintain his sugar. After 2 days at Northridge, we realized something more serious was going on and labs were drawn and that was when we realized he probably had the hyperinsulinism. We were then transferred to UCLA, a much larger hospital with pediatric endocrinologists, where the workup continued. He was started on diazoxide, which did not do much and then octreotide. We had our PET scan that indicated a focal lesion in the head of the pancreas, a genetic test that showed a paternally inherited abcc8 mutation, and so we ended up being transferred to CHOP for surgery when the local surgeons did not feel comfortable trying to do a surgery there. At CHOP, we went into surgery expecting to have a cure. During the surgery, Dr. Adzick couldn’t find a focal lesion and so he did several biopsies from the entire pancreas which revealed that Ezra actually had diffuse HI. It was a big blow, but the doctors there felt that we could manage his disease medically and so they did not remove anything and instead placed a g-tube. After a few more weeks, we finally had a regimen that worked to maintain his sugars: twice daily octreotide and overnight D20 in his tube.
Ezra has done fantastic since leaving the hospital nearly 2 years ago. We have not had any admissions and his blood sugars really have done well. Even though we did not find his HI for 5 months, his development has been normal. He runs, climbs, and talks up a storm, trying to keep up with his older siblings. At first, I was very nervous about what our life would look like, having a child with some extra needs. But everything has become second nature. My 4 year old daughter loves to help check Ezra’s blood sugar, and for the most part he doesn’t mind getting pokes or shots. We took a 2 week camping trip last year and brought all our D20 with us, and are looking forward to another trip this year.
How did it feel, both as a parent and a doctor, to be told that your child has hyperinsulinism?
Like many doctors, I had never actually heard of HI until my son was diagnosed. I trained at a community hospital and never saw it in medical school or residency. The doctors at UCLA were great and brought me a lot of good review articles to read so I feel like I have quickly become somewhat of an expert, probably like any parent of a child with a rare disease. I will keep reading and have enjoyed all the articles CHI links to on the facebook page because it helps me keep current with the latest research. While we were in the hospital, people often said it must be hard to be a doctor and the parent of a patient, but I feel like it has only been an asset, since I already had a basic understanding about glucose metabolism and the function of insulin.
What else can be done to raise awareness of HI?
For me, I want to make sure that the residents I teach at least have heard of hyperinsulinism, even though they will never understand all the details of the disease. I also try to stress that hypoglycemia is the most common preventable cause of brain damage in the neonatal period and that it needs to be taken seriously. And any hypo after 72 hours needs to be worked up more extensively. For parents who are not inside the medical community, social media is a great way to show what life is like for those affected.
What are the biggest challenges for you in parenting a child with HI?
Trying to navigate all the normal challenges of parenting with the added complications relating to hyperinsulinism. For instance, Ezra has always been a good eater, but like any toddler he is at a much pickier stage right now and often eats two or three bites of dinner and wants to be done. My older kids might get a treat after dinner if they finish their veggies. I don’t want to encourage Ezra’s pickiness and let him jump straight to dessert, but he also needs more sugar than my other two and so trying to find the balance there is hard. Whenever he does something different, I always wonder if it’s related to the HI or just something he does different because that is who he is. Overall I think lots of things are just more stressful. I’m already dreading sending him off to preschool.
What has the HI Family community meant for you?
When we were hospitalized in UCLA, it was clear that the only people who knew anything about HI were the endocrinologists. No one else had ever seen it before. None of the other parents I met in the hospital knew anything about it. Then we were sent to Philly and one of the first days we were there we met several other families with affected children who were also there for surgery and knew just what we were going through. Seeing so many families with children who are flourishing and grown has been a real encouragement. It is also nice to trouble shoot problems and get advice from others who have gone through the same thing.
You mentioned in your original post, “Everyone loved that you included personal photos.” Can you elaborate more on the importance of the patient role in research?
It is one thing to read a dry textbook definition of a disease, and quite another to see what a real, living, breathing human’s experience with that disease looks like. There are certain diseases that I only came to understand as a physician when I had a face to connect to the pathophysiology I learned about. Just being willing to share your story is a powerful way to help physicians and researchers understand why finding a cure and better treatments is such an important task.
In your presentation, you listed pre-existing maternal diabetes, pre-eclampsia, and babies large and small for gestational age as triggers for checking glucose levels in newborns. However, many newborns with HI who do not have these risk-factors do not have their blood sugar level tested. What advances would you like to see in a newborn screening process for hypoglycemia to prevent brain damage and death in newborns with HI?
Neonatal screening is a constantly moving target and even between the birth of my oldest and the birth of my youngest, new things were included. I actually think the Pediatric Endocrinology Society has excellent guidelines about testing. As a family doctor, I would defer to the judgment of people like Dr. Charles Stanley and Dr. Diva De Leon who have spent their entire careers studying this disease. A single blood sugar check prior to discharge may not help everyone. There are patients it would help, but there are also patients who might have a normal blood sugar at that check and then bottom out a day or two later. I think the most important thing we can do is educate people that HI exists, and if there are any symptoms of hypoglycemia in a neonate, even if they don’t have any risk factors, we should have a very low threshold for checking a blood sugar. I would love to see more research in this area as well as to the best way to make sure these cases are not missed going forward.