Because Prolonged Hypoglycemia is the Leading Causing of Preventable Brain Damage
Congenital Hyperinsulinism International (CHI) – dedicated to improving the lives of people born with the rare condition, congenital hyperinsulinism (HI), has launched the Be My Sugar campaign leading up to the 2016 Rare Disease Day. Here you will find the CHI Be My Sugar Gallery where you will find the beautiful faces of our Sugar Babies and you will learn about their experiences and lives in the words of their parents.
Babies born with HI, Sugar Babies, overproduce insulin, which causes low blood sugar. Prolonged low blood sugar can cause brain damage and death.
The terrible consequences of prolonged hypoglycemia are 100% preventable if Sugar Babies are diagnosed and treated in a timely manner. Families with HI babies also need long-term on-going support as treatment is complicated, constant, and prolonged. Be My Sugar is a call to action to support the needs of people born with this rare condition because sugar is life for Sugar Babies.
The CHI Be My Sugar call to action is:
- Raise awareness of HI to save lives and prevent brain damage
- Support research leading to better treatments and a cure
- Support access to lifesaving treatment, physicians, and supplies for every child born with the condition
- Support the global community of families living with HI
Each day leading up to Rare Disease Day, CHI has blitzed social media with a photo of a beautiful Sugar Baby in a Be My Sugar frame, and shared a story or a message from an HI family somewhere in the world. HI Families from 39 countries are a part of the CHI network.
The Be My Sugar campaign has been created to shine the spotlight on this rare condition to save lives and prevent brain damage. Prolonged hypoglycemia is the leading cause of preventable brain damage.
Please note: we’ve moved some of the profiles here to our HI-Stories section; please check there for more stories about our Sugar Babies and their life experiences.
Lewis
This was my son Lewis. We discovered at birth that he had hyperinsulinism. He stopped breathing shortly after he was born and his sugar was so low it wouldn’t register. He came home from the hospital after 3 week and was taking diazoxide and chlorothiazide. After a year he was weaned off the medications and had regular check-ups and was discharged from clinic just 2 weeks ago. He is 7 now and shows no symptoms.
Dhara
This is my baby girl Dhara. She is now 2. She was born by C-section. When she was born, she was very big and swollen, but nobody seemed to notice anything! Later, on the day she was born, I noticed her making noises and sweating, and I asked a nurse if this was normal. The nurse kept an eye on her, and a few hours later she was lying there lifeless, and she could barely open her eyes, so I ran to a get a nurse. The nurse checked her blood sugar and it was 0.2 mmol/. The nurses panicked and took her to the ICU unit. She stayed until she was 5 months old. Many tests were run on Dhara and they tried many medications. Finally, she stabilized. We were told she had one of worst cases they had seen in Glasgow, In 4 years. As a result of hyperinsulinism, she has had numerous seizures. She had one a few months ago. As she gets older, she isn’t a great eater. She takes diazoxide three times a day, and she has a subcutaneous infusion of octreotide through an insulin pump. She also has Maxijul added to her drink. She is now under the care of the Royal Manchester Children’s Hospital. They are now trying her on a new injection that is hopefully going to mean that after sometime, she can have the pump removed. If that doesn’t work, she might need an operation. She is such a bright and happy wee girl. You would never know what she goes through on a daily basis. It has been a hard two years but I am very proud of her. Fingers crossed that she grows out of this or that an operation will make it easier to manage.

Sameer Rai Kaul
This our sugar baby Sameer Rai Kaul. He is 5 years old. When Sameer was born he stopped breathing and was rushed to the NICU and they had discovered his blood sugar had dropped dangerously low. After several days in the NICU he received continuous IV feeding, special formula and numerous blood draws they diagnosed him with hypoglycemia. They didn’t know the cause of this and began diazoxide treatment for two months when he returned home. After these initial 2 months he began weaning off the diazoxide and was able to maintain sugars in the 70-80s. Sameer has had no other issues with this disease and is a healthy almost 5 year old.
Kevin
This is my 8 year old son, Kevin Jr. He was born with hyperinsulinism. He is an outgoing, smart, caring, loving, handsome young man. He loves basketball, baseball, his 2 puppies, and his whole family. Last school year during spring break, he got type 1 diabetes added to what he already had. My husband and I love him so much and are so proud of him. He will be 9 on June 9.
Finn
Finn decided he needed to be born about 6 weeks early, and we soon found out why: He had a tumor growing in his liver that needed to be removed ASAP. His sugars didn’t even register at birth, but the tumor consumed everyone’s immediate attention and so he was put on dextrose to keep them up until the tumor was removed. We lived in the Chapel Hill Children’s NICU and slept at the nearby Ronald McDonald house as he healed from the removal of the thankfully benign mass on half his liver.
Once he recovered, the research into his low sugars began. The doctors suggested all kinds of scary diseases and syndromes but finally, after contacting CHOP, nailed it down to hyperinsulinism. We were sent home with an NG tube and a regimen of diazoxide, feedings and continuous dextrose. His sugars remained low, however, so after a stay in the closest hospital with a pediatric endocrinologist he was flown to CHOP. There we learned that his case was a rare type of the already rare disease. After much deliberation he had a G-tube placed and after recovery and regulation we were sent home with a new regimen and a lot more knowledge.
He’s had ups and downs since then, but to play and talk with him you wouldn’t know he has any problems. He’s full-speed-ahead, and wearing his feeding pump backpack has only made him stronger; he even helps daddy move furniture! His “tubie”, “beeper” (continuous glucose monitor) and glucometer have always just been a part of his life and he takes it all in stride. He’s happy to show his tube to his friends (and completely healthy sister) and tell them about it. He is such a blessing and joy to us!
Loralye
Loralye was born full term, with no complications and she did not have critically low glucose levels. However, just weeks after her first birthday, she had a horrifying seizure and became unresponsive while rushed to the Emergency Room. Her glucose level was a mere 13 and I was told my daughter MUST HAVE overdosed on diabetic medications. My “Peanut” was limp, sweaty, clammy and shaky, yet they wanted to send her home!? I insisted she be admitted for observation and after 24 hours they confirmed she had NOT overdosed and 24 hours later, she was diagnosed with congenital hyperinsulinism, and we later learned it was caused by an ABCC8 gene mutation.
In an instant My life revolved around numbers, nutrition and needles; all for a toddler, whose favorite word was, NO! Loralye tried Diazoxide, Diaril and even raw, gritty cornstarch, but nothing seemed to work to stabilize her glucose. Dr Thornton needed fasting studies, labs and scans to devise a plan of care. Peanut and I stayed busy w ultrasounds, PET scans, labs, poked every 2 hours, multiple IVs and PICC lines. Then she had surgery, which lead to an epidural, catheter, more IV tubes, a feeding tube and a lot of pain. But it was all worth it when she was deemed CURED about a year later!
Nate
Sending out a BIG hello to all from sugar baby, Nate & I. Nate was born with Pierre Robins Sequence, but there always seemed to be something else lurking in the background that we couldn’t put our finger on. At 6 months old Nate suffered a convulsive seizure, as a result of extremely low blood sugar… And that was it. One minute I was making an early morning Sunday coffee and the next we found ourselves initiated into the world of hyperinsulinism (HI).
It’s been a steep learning curve, so far. Some days are FABULOUS. Other days the term ‘day’ itself seems too long a time frame, too far away to achieve, so we break it down into hours, sometimes minutes. Our lives are ruled by the clock, checking blood sugar levels, feeds & meds. Yet through all the ups and downs there is one thing that has remained constant and that is my beautiful little Nate. He is the same courageous, loving and happy little boy he was before HI, and his strength and cheeky character continue to blossom in spite of it.
No matter how unwell he is, you can guarantee Nate will be smiling, his wonderfully contagious smile, to everyone in his view. I couldn’t be prouder of my Sugar Baby and I’m honored to have been chosen to be his mum.

Julieta Joy
My sugar baby is Julieta Joy, she was born with an 18 blood sugar last summer. We were lucky enough that they checked her blood sugar as soon as she was born because she was unresponsive. She was diagnosed with hyperinsulinism when she was 5 days old, and she struggled in the NICU for about 3 months until we could stabilize her sugars and bring her home.
She currently eats high caloric formula through a g-tube every three hours and has to eat continuously overnight for 11 hours to maintain stable sugars. She also gets two injections twice a day. She is now 7 months old and is growing and meeting her milestones.
We hope that she did not have any brain damage due to her low blood sugars early on. She is the perfect baby, and transmits nothing but love to all around her. Her HI is non-genetic so we hope that she will someday outgrow this very difficult rare disease.

Jeremiah
This is Jeremiah. He is five years old and has no known mutation. He was diagnosed at 11 months old. Only on the 4th visit to the emergency room, after having is 4th seizure, was he diagnosed. When I brought him to the emergency room, after his second seizure, we were told he was just having night terrors. Then he was diagnosed with epilepsy, and finally with HI. His condition is managed with diazoxide and diet.
Aapo from Helsinki, Finland
Our son Aapo was born in February 2015 in Helsinki (Finland). 34 hours after birth his low blood sugar was noticed – he spent three weeks at the NICU in Helsinki and was diagnosed with hyperinsulinism. He has a mutation in the gene HNF4a1 and is diazoxide responsive – in September 2015 he was weaned off and is now cured! His gene mutation may cause diabetes later in his life. We are very grateful for all the great support we have received from the HI family during our journey and we hope our story will encourage other HI parents.
Ezra
Ezra was diagnosed with HI at the age of 5 months after a seizure. Although initially we thought he had focal disease, during surgery we discovered it was actually diffuse. He is currently being treated with octreotide injections during the day and overnight dextrose while he sleeps. He is a sweet and active 14 month old who is adored by his older siblings. We are so thankful he is a part of our family.

Kieran from Wisconsin
This is Kieran. He was diagnosed with CHI after a hypoglycemic seizure. He was hospitalized for two weeks at the Children’s Hospital of Wisconsin until he was diagnosed. He has a mutation in UCP2 and is responsive to diazoxide. He still struggles with low blood sugars and the affects of spending the first 12 months of his life with low sugar, but he is stubborn and determined not to let anything slow him down!

James and Matthew from New Jersey
We are from New Jersey and both our sons were born with transient hyperinsulinism. They were treated at the Children’s Hospital of Philadelphia (CHOP) where they both were put on a course of diazoxide and diruil. Both resolved after 5 months of treatment. Neither child carries the genes for HI, nor do my husband and I. I did not have gestational diabetes or hypothyroidism.
James, my oldest, was an emergency C-section and needed to be resuscitated at birth. The nurse who took care of him decided to check his sugar, so he was monitored since birth – we feel very lucky about that. Doctors at our local NICU could not figure out why his sugar wasn’t resolving so after a few weeks we were transferred to CHOP where he was diagnosed and treated for HI.
When I became pregnant with Matthew we were so worried he would have it too, but were assured he wouldn’t because there was no genetic cause. But, to be safe, we would check him when he was born. Unfortunately he was born with transient HI as well. CHOP’s first case of sibling transient hyperinsulinism. It was a rough start for both our boys but we are grateful that they recovered and are currently doing very well. Thank you for letting us share our story.

Leo
This is our 19 month old sugar baby, Leo. At 4 months old, he had a seizure and less than 3 days later, he was given the diagnosis of hyperinsulinism. We are very fortunate that he responds well to diazoxide and on “good” days doesn’t require more than 2 or 3 blood sugar checks. He has a mutation on the UPC2 gene, inherited from his father, who is non-HI. Apparently, there are less than 10 reported UPC2 gene mutations worldwide and the particular region of their mutation has never been reported before. We are traveling to CHOP in the very near future so Leo’s father can participate in a study as it relates to the UPC2 gene. We are excited for the opportunity to learn more and to contribute to the ongoing research regarding this very rare disease.
Leo is a happy, charming, silly little boy who takes his medicine like a champ and barely flinches during his blood sugar checks. He is a brave little guy who never ceases to amaze us each and every day. There have been some dark days in dealing with this disease, especially in the early days and it can be challenging when he’s not well or is being a picky toddler….but we feel truly blessed. We also feel incredibly grateful and blessed for the CHI Parents Forum; it is an incredible thing to be able to connect with other parents, worldwide, who can relate, understand and show support.

Ashlee
My name is Ashlee and I was diagnosed with HIHA when I was about 14 months old. I have always had to check my blood sugar many times each day, watch the amount of protein I eat and take a lot of medicine. It is really frustrating sometimes because I crave all of the foods that I should not eat.
My parents and I do a lot to advocate and help others with this disease. I have even tried new medicines in hopes of it helping manage my blood sugars. I think that living with this disease has helped me become really understanding and empathetic about people dealing with rare diseases.
I want to be a nurse and next year, when I am in 11th grade, I will be starting an early college program to start my nursing program prep. I told my mom that I dream of being a pediatric nurse for either CHOP or Cook Children’s Hospital and working in their hyperinsulinism clinics. They think that is a great goal for me to have!

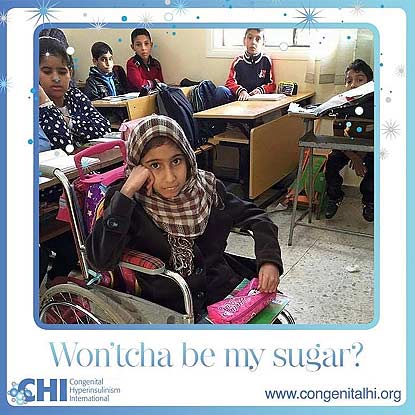
Fatima from Benghazi, Libya
This is beautiful Fatima. She lives in Benghazi, Libya where she lives with her loving family. Fatima is in a wheelchair because she cannot walk, the result of prolonged untreated hypoglycemia before she was diagnosed with hyperinsulinism hyperammonemia syndrome. Also, due to hypoglycemia, Fatima has trouble with her jaw and esophagus. Fatima wishes for a cure for hyperinsulinism hyperammonemia syndrome. Fatima loves to learn, reading and writing.
Asher from New Jersey
Hi everyone! This is my son Asher! We are from New Jersey! Asher was transported to the Children’s Hospital of Philadelphia where he was diagnosed with KATP defect with Diffuse Congenital Hyperinsulinism and Beckwith Wiedemann Syndrome, at only 2 days old! He had a near-total pancreatectomy (98%), appendectomy, and a fair share of tests done during my his month of life.
This has been quite an adventure for us. I cannot wait to see what the future holds for this little guy! He is already doing amazing things. He is one of the happiest babies that I know. I am very thankful for CHI, bringing all of these families together. Asher and I have made some wonderful friends! We wish all of the best to all of our fellow HI babies and families!

Harley from Australia
This is Harley from Australia. He was diagnosed with hyperinsulinsim at 4 months old. He is now 2.5 years old and not letting it slow him down. He is currently on diaxoxide to help keep him stable. Harley is always smiling and happy. He is a very determined little man who is always eager to explore and try new things
Paula from Catalonia
Paula is from Catalonia in Spain, near Barcelona. She has two mutations in the gene ABCC8. She has has taken diazoxide since she was two days old, although she has only a partial response to it.
We’ve had four years of very hard times, but we have also learned that the brightness in her eyes, is the biggest strength.
From her diagnosis, we have discovered many new words such as hyperinsulinism, dextrose infusion, diazoxide, ocreotide, pancreatectomy, gastrostomy, PET scan… although none of us wanted to discover them.
But we’re very thankful to the CHI family, it’s great to have friends that know exactly what you’re feeling, or what you’re worrying about, no matter where they live.

Marlee from Australia
“Hi, I’m Marlee and I’m from Australia! I’m 2.5yrs old and was diagnosed with hyperinsulinism at about a week old after giving Mum and Dad a huge fright as we were getting ready to head home from the hospital.”
“It’s been a rough ride since I was born but I am still one of the happiest, smiling kids you’ll meet.”
“I have to take a medicine called diazoxide to try and keep me stable and Mum or Dad checks my blood sugar levels anywhere from 3 times a day up to 10 or more on days where I’m not feeling the best and things become unpredictable.”
“The doctors don’t know really what the future brings for me and my hyperinsulinism so we just take each day as it comes and hope that things remain stable for now.”
“We are so grateful every day for all the support and love we get through CHI. Families from all around the world have made living with this condition much less isolating and just that little bit more bearable.”

Maxwell
Hi, I am Maxwell! I will be two years old in May, and I have hyperinsulinism/hyperammonemia (HIHA.) My blood sugars are managed by a high diazoxide dose and diet. I like to keep my family on their toes because my blood sugar drops when I’m teething and when I get sick, which has led to some extra hospitalizations. I have such a happy, easy going personality. I love keeping up with my big brother and snuggling my dog.
Penelope
Penelope was born with meconium aspiration that required ECMO treatment and during recovery we discovered she had ‘blood sugar issues,’ that turned out to be congenital hyperinsulinism (HI). She responded well to diazoxide and it later transpired after further testing that her HI was the result of Beckwith Weidemann syndrome. It is particularly difficult for babies with both as it is quite a small cross section and can be overwhelming dealing with not one, but two rare diseases! Penelope is currently being trialed off diazoxide and is doing great so far!

Olivia from Texas
I found out something was going to be wrong with Olivia two weeks before I had her, but nobody knew what. On December 18th, 2013 Olivia was born with a blood sugar of 4. Since then I have literally felt my heart break, but at the same since, my heart has never felt so much joy.
In 2 years, Olivia has stopped breathing on me more times than any parent should have to experience. I have seen the worst. Olivia had 98% of her pancreas removed in January 2015. After her surgery, Olivia had problems with pain and keeping her airway open. I spent a lot of days in the PICU in Texas. I knew this is what rock bottom felt like. On our 3rd day in the PICU the nurses started shutting the curtains all around us, but ours had a little sliver still open, and I saw that another little one did not made it (for different reasons), yet I was still holding Olivia, and she was fighting. I knew from that day, I need to keep fighting for this little lady, because she has hit rock bottom, and has kept fighting. Olivia has two rare diseases hyperinslinism, and Kabuki, neither one of which, I would wish upon someone. Olivia still suffers from HI even after the surgery. Olivia still take meds for low blood sugar, she still needs her blood sugars checked throughout the day. Olivia has to eat every 3 hours, and still needs to be on continuous dextrose at night.

When Olivia was born all I wanted was some answers: was she going to walk? Would she ever eat on her own? Would she be able to talk? Nobody was ever able to answer these questions. I was told “take it day by day, and celebrate each milestone she hits.”
Now Olivia is almost 26 months old, she is walking, she is eating on her own, and she is trying to form words.
Hyperinsulinism has changed my life, I have lost a lot in 26 months, but I have gained so much more. I see the world differently, people differently. I understand the saying, “It takes a village to raise a child.”
Alyssa
Alyssa is our 9 year old sugar baby! She was diagnosed at 10 months old and has been on the medication, diazoxide, since then. Alyssa was named 2015 Salem County Children’s Miracle Network Ambassador. She has ridden in a few parades raising awareness for congenital hyperinsulinism. Alyssa is such a brave, strong little girl and she lights up our life with her beautiful smile!

Evelyn
This is my sugar baby Evelyn. She spent the first few weeks of her life dealing with low blood sugars in the NICU, which led to her diagnosis of hyperinsulinism. Evelyn also had aspiration issues which led to another harrowing hospitalization where we learned she could not swallow thin liquids. An NG tube was placed, and she was put on oxygen in order for her lungs to heal. The issues continued to add up, which led the team of doctors to suggest genetic testing. We wouldn’t learn of her mosaic Turner syndrome until she was 4 months old. At the time of her diagnosis, her geneticist could only find one other documented case of hyperinsulinism and mosaic turner syndrome. The continued feeding difficulties, and overnight feeds needed for blood sugar management led to a g-tube being placed at 4 months old.
Evelyn is managing her HI well on diazoxide and g-tube feeds. Despite all of her difficulties, she is alive and thriving. She is a happy, smart, energetic, loving 3 year old.

Annika June
“Hi, I am Annika June! I was diagnosed with congenital hyperinsulinism (HI) diffuse disease at two and a half months old. After being transferred from our hospital in NY to CHOP, I had a 50% pancreatectomy and g-tube placed.”
“Now, that I am two years old, I keep my blood sugar levels up with frequent meals and snacks during the day and continuous dextrose through my ‘tubie’ overnight. My favorite things to do are playing with my big brother and blowing bubbles!”

Gracie from Lubbock, Texas
This is Gracie from Lubbock TX. She is now 6 years old and still dealing with developmental delays and challenges. She was diagnosed at 4 months old. Her symptoms appeared hours after birth but the nursery mistook it for transitional diabetes and sent us home … my only wish is for hospitals to stop discharging any infant showing any kind of signs of hypoglycemia, even if it could only be transitional diabetes … keeping her longer in the hospital could have meant a chance at a normal life … comparing Gracie’s development to her younger sister’s shows how much of a deficit Grace has … early diagnosis could mean less brain damage, and seizure history or epilepsy would be less likely … ALL BABIES DESERVE THAT MUCH!

Ava
This is my sugar baby..Ava had a rough start in life but she is now nearly 7 years old and managed solely by diet and her pump at night. We are so proud of the way Ava handles her condition every day.She is amazing and we love her very much!

Joslyn
Joslyn Gabriella is our one and only sugar baby! Lately it’s been a struggle keeping her blood sugar levels up. But now it’s looking better and her doctor is even considering lowering her dose of diazoxide. Joslyn is one very strong and determined little girl and we pray every day that she’ll outgrow her hyperinsulinism.

Juliana
I am Juliana Elizabeth, 20 months! I am still on this HI journey and my low sugar continues to be managed with Diazoxide. I continue to have my sugars checked daily and follow-ups at CHOP. I also have a few other medical issues that I am told don’t all relate to my HI … doctors say I am one of a kind … my parents say I am their perfect little girl! Most people think I am 2-3 years old between my long hair and how tall I am, but I am still only a year old! I like to do puzzles, color, run around and play with my older brother, Justin. I also LOVE “coco” (what I call chocolate), but that’s okay if I eat sweets because I am a Sugar Baby.
It is important to continue to spread awareness of HI, the rare disease I and others have, as well to educate people to prevent the serious side effects it can cause if not properly diagnosed early on and treated.

Kinley
Kinley – my little sugar baby! It is believed that her hyperinsulinism is resolving, and she is thankfully now medicine free. However, lately it seems that maintaining her blood sugar at a safe level is a daily struggle. She is such a strong, beautiful and resilient little girl.



Adi
September 7th, 2015, week 36, contractions, at the hospital I was rushed to an emergency C-section. A beautiful baby girl was born to the world!
At the recovery room your father, (a doctor himself), had told me your sugar level was low and you were to stay to be monitored for a couple of hours before being brought to me. Your sugar was 22 and insulin level 14. At Shaarei Tzedek hospital, based in Jerusalem, ALL babies’ sugar levels are regularly checked at birth. Couple of hours turned into 24 hr in the NICU. I was even too week to come and see you. After what seemed like forever your daddy wheeled me in to see you and placed you in my arms. So beautiful and calm. Your hospitalization stretched out to be a month long hospital stay at the NICU. At times we were not allowed to even touch you, for the week you had received high levels of glucose through your umbilical artery because the dosage through the vein was just not strong enough. So we sat by your side and sang and sang for hours long so that you could at least hear our voices.

Before being discharged your dad ran from pharmacy to pharmacy to try and obtain the Diazoxide, baby calorie, hydrochlorothiazide- so that once you were ready to come home – it would be soon as possible with any further delay. This was no simple task. You will grow to learn just how unique you are. In and out. CHI is a rare genetic disease and the medications used are not commonly found.
When you came home, what a joy- your sister and brother were thrilled you had finally arrived.
As for your father and I, we were full of concern and worry for you. Your father coming from the medical field, more so than I, being a physician, he knew the potential complications, the intensity and the importance of being on top of things. I was more at the bliss of ignorance stage. I had cried a lot the first month you were born, prior to the final diagnosis, hoping, praying that this would all be transient, that your sugar levels had dropped wishfully due to the gestational diabetes I had during your pregnancy. Hopefully this would all be a passing nightmare which we would all awake from and you would be a normal baby with a normal life – not being pricked every couple of hours, often woken up to be fed, have devices injected into your frail gentle body so that we can constantly monitor your sugar level to prevent possible brain damage – this is not the life we had planned for you.
Now that the blood test has confirmed the worst of our fears- Persistent Hyperinsulinemic Hypoglycemia of Infancy- we had to deal with the situation. For your father, difficult as it may have been, all you had to do was smile your big gorgeous smile, and we knew it would all be ok. Ups and many downs but we will give you our very best. Life has changed us since you came to our life and we are so thankful for that! We thank God for having chosen your dad and I of all people to be your parents!!!
Running from endocrinologist, to weekly physical therapy due to your hypotonia and currently working on getting an appointment at the eating disorder clinic. Didi, we are trying to give you the best possible care and are thankful you were lucky to be born in an era with abundant medical knowledge which hopefully will advance even more, speedily, for your benefit.
When your sugar drops, the sensor on your body has a mechanical error, a medication bottle falls and breaks- we lose more than a heart beat and I am unable to function at least till the next morning. and when the new day comes, it brings with it new energies for hopefully a new and wonderful day, challenging as it may be. The following words from Bruno Mars’s song “Just the way you are” were not intended for you ,but at a simple glance suit you so perfectly. Slightly changed, this is dedicated to you my love, your capturing smile that you throw to just anyone around you, your awesome eyelashes that don’t go unnoticed and the positive light and energy that just shine from you!
I love you,
Mommy
“Just The Way You Are”
Oh, your eyes, your eyes
Make the stars look like they’re not shining
Your hair, Your hair
Falls perfectly without you trying
You’re so beautiful
And I tell you everyday
Yeah
When I see your face
There’s not a thing that I would change
Cause you’re amazing
Just the way you are
And when you smile
The whole world stops and stares for a while
Cause, girl, you’re amazing
Just the way you are
Brenna
When you find out you are expecting a child, your thoughts immediately turn to expectations. What will the baby be? A boy? A girl? Will the baby look like you or me? Take after my side of the family or yours? Have my curls and your red hair? Have my gutsy laugh and green eyes and your smile and good sense of humor? Will our baby grow up to be a teacher? An artist? A politician? A Nobel Prize winning scientist? The possibilities were as infinite as the limits of the love I felt for this being that we created but had never met.
One day in September 2007, we embarked on the journey of finding answers to all of those questions when our daughter, Brenna, was born weighing 6 lbs 15 oz at 5:17 AM on a beautiful day at the Jersey Shore. By the OBGYN’s account she was born 10 days early but I knew she arrived right on time. She had the most adorable pudgy cheeks but was very difficult to feed. Several hours after birth she didn’t seem to prefer formula or breastmilk, slept A LOT and ate VERY LITTLE! I just felt like something wasn’t right. She had hypoglycemia (low blood sugar) after birth and had some tremors but was misdiagnosed with having an immature neurological system. She was admitted to the NICU where they collected samples that were sent off as part of her newborn screening and she spent 3 days in the NICU on a dextrose drip and regular bottle feedings. After her blood sugar levels stayed above 65 they weaned her off the drip, told me to feed her every 2-3 hours and sent her home with me. I asked if I should get a glucometer and monitor her blood sugar but the neonatologists responded to me like I was a hysterical, first time mom. “No, take your healthy baby home and enjoy her.” they said.

The first six months were as anyone would expect … sleep deprived yet blissful. Yet there was one small problem. She was very difficult to feed. It would take hours for her to consume just a few ounces of formula and when she did eat, she’d spit up most of what she drank. So, after repeated trips to the pediatrician where they assured me that she was healthy, growing and developing normally, they told me to change to a more sensitive formula. They, too, told me to “take home your healthy baby and enjoy her.” Not left with a lot of choices, we tried many brands and varieties of formula in an effort to find one that she would not spit up as much and as frequently, to no avail.
Six months after she was born, in March 2008, she had a seizure right in front of me. It was the first one I’d seen and recognized immediately as a seizure. God only knows how many she had that were unrecognized or not seen. Words cannot express how incredibly scary and devastating it was to witness that! After talking her through the seizure, she was alert and responsive. So, I picked her up and woke my husband to tell him what just happened. He called the pediatrician to seek his advice. While he was on the phone, I wanted to see if she would take a bottle. I fixed a full 8oz bottle, sat in the recliner and fed her. She drank the entire 8oz bottle in less than 15 minutes, without fussing or spitting up. The pediatrician said he wanted to see her. So, we packed up and drove to his office. When we got there I told him the one thing that seemed off to me was how she consumed a full bottle for the first time in six months in a short amount of time without crying or spitting up most of it. He told us to take her to a children’s hospital of our choice.
We stayed with Brenna for two weeks at a children’s hospital in New Jersey but the doctors there couldn’t figure out what was wrong with her. Over the first week, I kept in constant contact with the pediatrician and told him everything the specialists were telling us. It was our pediatrician who first said the word hyperinsulinism (HI) to me. He explained that he had consulted with some colleagues and poured over my maternity records and her medical records from the hospital, spoke to them about Brenna’s condition, did some of his own research and thought she might have it. He admitted that he had never personally treated a patient with hyperinsulinism in his 30 years of practicing medicine but he was sure that was what she had. To our knowledge her newborn screening had come back normal with nothing to report. However, much to our dismay, it did not include a screening for congenital hyperinsulinism. So, he urged me to research this condition in the computer library for families in the hospital.
After reading some of the information my family and I found on the internet, I begged to be transferred to the Children’s Hospital of Philadelphia (CHOP) After days of waiting for an available bed and transportation we were on our way to Philadelphia. Upon admission, the CHOP HI team was explaining how they were planning to investigate what was happening to our little girl. A few hours later, they checked her vital signs and her blood sugar. To our surprise there was no need to wait, it was already low enough for them to administer a Glucagon injection and find out if Brenna had what they suspected, congenital hyperinsulinism. Moments later, their suspicion was confirmed. Once we received a diagnosis, reality set in and I did what any mother would do. I began the inquisition. The barrage of questions must have seemed limitless like the wonder I felt when I first learned I would finally become a mother. The expectations that I dreamt of when I first learned I was pregnant were quickly replaced by a litany of other questions and a torrent of emotions and that spilled out of my mouth and tear ducts in an emotional rage like a scene worthy of Shirley MacLaine in Terms of Endearment or Sally Field in Steel Magnolias. Why did this happen? What did I do to cause this? Why didn’t they catch this before she was born? Why didn’t the neonatologists and pediatrician screen for it or catch it when she was born? Would she live or die? Would she grow up healthy and act like a normal or average child and live a happy childhood? Would she be able to walk? Talk? Play sports? Would she go to school? Would she be able to drive a car? Would she graduate from college? Would she be able to get a job and become a productive member of society? Would she ever get married? Would she be able to run a marathon? Would she be able to have a baby of her own?
You name it, I asked it and they were only able to answer some of the questions with certainty. The rest we would have to wait and see. Then the flood gates opened. I expressed myself in true gut wrenching fashion that would have made Shirley and Sally proud. I spilled forth every emotion fathomable from the relief and gratitude that we had an answer and a plan, anger that she was not properly diagnosed at birth, when taken to the NICU or released to go home, heartbreak that she would live with this condition for the rest of her life, fear of the unknown impact of her condition caused by six months of chronic hypoglycemia and the stigma of that she would later face as the unknown developmental consequences and the side effects of the necessary lifesaving drug took effect, worry about the life long effect of this medicine on her other organs and whether she’d ever be able to have a child of her own someday, regret for failing as her advocate and not following my first instinct to test her blood sugar after discharge from the NICU anyway, frustration over not being able to get her pediatrician to listen when I repeatedly expressed my concern about her eating habits or lack thereof, and the deepest sorrow that she may not ever be the discoverer of world peace or the cure for cancer grief that the healthy baby I was told to take home and enjoy was in fact not healthy.
The doctors and nurses stood there, silent, patient, listening to every word, consoling me and some crying along with me. We stayed another two weeks while Dr. Charles Stanley and his hyperinsulinism team determined that Brenna had what is known as diffuse HI. They started her on an oral suspension called diazoxide. After a few days they conducted a safety fast to see if the dose of this medication along with eating solids and drinking formula would keep her blood sugar stable. The fast was a failure. She did not fast as long as they wanted. Then, it was determined that the diazoxide, coupled with her food intake, was not enough to sustain her blood sugar at safe levels. So, they added Octreotide and later added diuril due to the fluid retention caused by the high dose of Diazoxide, a drug that she would need for rest of her life. The staff at CHOP told us about their partnership with the University of Pennsylvania and explained they could offer her a diagnostic tool, a PET scan.
We met their world renowned expert surgeons who could determine if her HI could be cured by removing part of or her entire pancreas rendering her a diabetic. We opted to take a conservative approach as she was stable and responding well to the medicine and they agreed and asked us to participate in their research study. They were collecting DNA samples and sending them off for genetic testing that would hopefully lead to an explanation. We gladly agreed to participate in the hopes that we would be able to cure Brenna of this disease. My pregnancy was uncomplicated with no Gestational Diabetes. However, I did have pre-eclampsia and thus was induced. I had a normal, drug-free, vaginal delivery and there is no family history of hyperinsulinism in our families. So, we hoped that this test would unlock the mystery of how we got here. Unfortunately, after weeks of waiting, the genetic test yielded inconclusive results. We had no idea what part of her DNA was affected, whether she could pass this on to her own children or if we would have more children with the same condition. Since she continued to respond so well to the prescribed medications, they were confident that she was well enough to go home. In April 2008, Brenna was discharged from CHOP with prescriptions for diazoxide, diuril, octreotide and an emergency glucagon kit. We were also educated on how to check and monitor her blood glucose at home and given her first of many glucometers and test strips.
Three months after discharge from CHOP we had to stop the Octreotide when she had an episode of dangerously high blood sugar. Doctors at CHOP recommended that we eliminate the Octreotide from her regime because her appetite had somewhat improved with her curious palate that began to enjoy a variety of solid foods more than formula. In the spring of 2009 we started to become anxious and suspicious about Brenna’s developmental milestones. Brenna was a late walker and talker and still can take or leave eating (unless it was something she REALLY loves such as M&M’s, hot dogs, chicken nuggets…typical childlike fare). We had her assessed by speech, occupational and physical therapists and they confirmed one of our worst fears. She had significant delays in all three areas but they were confident that with their help, she could regain and overcome these deficits. So, we enrolled her in early intervention services with our local school district where she has undergone years of Speech, Occupational and Physical Therapy to combat the challenges of her developmental delays which she may live with for the rest of her life. To this day, I still relive the emotional roller coaster when our HI journey first began but in spite of all this, we are grateful. While Brenna has overcome much so much in the past few years, she still has significant cognitive and developmental delays.
Through it all she remains positive. She is funny, loving and sees the beauty and the best in everything and everyone. Sometimes, I get off the roller coaster long enough to observe our feisty little girl who is growing up and making strides and then I feel them. The infinite possibilities, and I immerse myself in the wonder. What will she become when she grows up? The answer is simple…anything she wants. While we don’t have all the answers we know one thing for certain she will always be her Mommy’s baby and her Daddy’s girl, just like we dreamed she would be.
Dante
Dante, the biggest of his triplet siblings at birth in Nov. 2014, weighed 2 pounds, 12. His brother Austin, was born at 2-7, and sister Tavianna, at 1-10. Dante was the first to leave the NICU, going home at 10 weeks old. He was gaining weight and doing well at home when, on April 24 he turned bright red, then blue, holding his breath and staring. He then took a couple deep breaths and his color came back. A blood test in the Emergency Room showed his blood glucose level at a dangerously low 35 mg/dL. Dante was immediately admitted and his lows were managed with IV dextrose while doctors searched for the cause. High insulin levels pointed to hyperinsulinism, and he was treated with diazoxide, octreotide and dextrose via a nasogastric (NG) tube, keeping his blood sugar steadily in the mid-60s. Doctors said he was ready to be discharged. By then, Kija’s own research showed her “CHOP was THE place for HI,” even though it was across the country from their San Diego home. She spoke with HI nurse who told her that CHOP’s protocols didn’t indicate discharge with sugar levels in the mid-60s. Then Dante threw up, dislodging the NG tube. Within 45 minutes, his blood level dropped to 37. “That’s when I told the doctor, ‘We need to go to CHOP.'” Kija says. “I wanted to know I brought Dante to the best place with the best doctors with the best knowledge.”
They came to Philadelphia via medical flight on May 22. Genetics testing indicated Dante’s HI may be focal (although it wasn’t the typical gene mutation), and an 18F-DOPA PET scan showed the whole tail of Dante’s pancreas “lit up like a Christmas tree,” Kija says. “We were joyous thinking it was focal disease and he could be cured by surgery.” But it wasn’t so simple. Surgeon-in-Chief N. Scott Adzick, warned it didn’t look like a typical focal lesion; the tail was too bulbous. “Dr. Adzick is the one who called it,” Kija says. In about 5 percent of PET scans, what appears to be focal turns out to be diffuse disease. Pathology didn’t show focal disease. Dr. Adzick ended up removing 40 percent of Dante’s pancreas.
Post-surgery, Dante still had low glucose. But the family and doctors decided on medical management vs. a second surgery for a near-total pancreatectomy. “With the tail, and its abnormal concentration of beta cells gone, we’re hoping he’ll be less effected by HI and even outgrow it,” Kija says. The original treatment plan was to give Dante octreotide during the day and continuous dextrose via a g-tube at night. But another twist presented itself: Octreotide made him vomit. So the plan was adjusted to continuous dextrose infusion along with tube feedings and bolus dextrose if needed. Kija was trained in how to manage the pumps, and they went home after a month at CHOP. While medically managing Dante’s HI is challenging — especially with two other babies around — it’s allowed Dante to maintain a safe sugar level and keep 60 percent of his pancreas, which could mean he won’t eventually develop diabetes and the life-long complications that come with it. “If we have to do something difficult for a few years for him to avoid diabetes, I’ll do it,” Kija says.
Since November, Dante has been able to tolerate two shots of octreotide a day, allowing him an eight hour window without all his tubes. “That lets him play with his siblings without us worrying about the cords getting pulled,” Kija says. “He is just taking his first steps.” Dante has had a couple of hospitalizations when he had a cold or stomach bug, which seems to compromise his ability to maintain his sugar levels. “He’s still a really happy baby — even when I check his blood 10 time a day,” Kija says. “He smiles all the time.”
Sameer Rai Kaul
This our sugar baby Sameer Rai Kaul. He is 5 years old. When Sameer was born he stopped breathing and was rushed to the NICU and they had discovered his blood sugar had dropped dangerously low. After several days in the NICU he received continuous IV feeding, special formula and numerous blood draws they diagnosed him with hypoglycemia. They didn’t know the cause of this and began diazoxide treatment for two months when he returned home. After these initial 2 months he began weaning off the diazoxide and was able to maintain sugars in the 70-80s. Sameer has had no other issues with this disease and is a healthy almost 5 year old.
Kevin
This is my 8 year old son, Kevin Jr. He was born with hyperinsulinism. He is an outgoing, smart, caring, loving, handsome young man. He loves basketball, baseball, his 2 puppies, and his whole family. Last school year during spring break, he got type 1 diabetes added to what he already had. My husband and I love him so much and are so proud of him. He will be 9 on June 9.
Finn
Finn decided he needed to be born about 6 weeks early, and we soon found out why: He had a tumor growing in his liver that needed to be removed ASAP. His sugars didn’t even register at birth, but the tumor consumed everyone’s immediate attention and so he was put on dextrose to keep them up until the tumor was removed. We lived in the Chapel Hill Children’s NICU and slept at the nearby Ronald McDonald house as he healed from the removal of the thankfully benign mass on half his liver.
Once he recovered, the research into his low sugars began. The doctors suggested all kinds of scary diseases and syndromes but finally, after contacting CHOP, nailed it down to hyperinsulinism. We were sent home with an NG tube and a regimen of diazoxide, feedings and continuous dextrose. His sugars remained low, however, so after a stay in the closest hospital with a pediatric endocrinologist he was flown to CHOP. There we learned that his case was a rare type of the already rare disease. After much deliberation he had a G-tube placed and after recovery and regulation we were sent home with a new regimen and a lot more knowledge.
He’s had ups and downs since then, but to play and talk with him you wouldn’t know he has any problems. He’s full-speed-ahead, and wearing his feeding pump backpack has only made him stronger; he even helps daddy move furniture! His “tubie”, “beeper” (continuous glucose monitor) and glucometer have always just been a part of his life and he takes it all in stride. He’s happy to show his tube to his friends (and completely healthy sister) and tell them about it. He is such a blessing and joy to us!
Loralye
Loralye was born full term, with no complications and she did not have critically low glucose levels. However, just weeks after her first birthday, she had a horrifying seizure and became unresponsive while rushed to the Emergency Room. Her glucose level was a mere 13 and I was told my daughter MUST HAVE overdosed on diabetic medications. My “Peanut” was limp, sweaty, clammy and shaky, yet they wanted to send her home!? I insisted she be admitted for observation and after 24 hours they confirmed she had NOT overdosed and 24 hours later, she was diagnosed with congenital hyperinsulinism, and we later learned it was caused by an ABCC8 gene mutation.
In an instant My life revolved around numbers, nutrition and needles; all for a toddler, whose favorite word was, NO! Loralye tried Diazoxide, Diaril and even raw, gritty cornstarch, but nothing seemed to work to stabilize her glucose. Dr Thornton needed fasting studies, labs and scans to devise a plan of care. Peanut and I stayed busy w ultrasounds, PET scans, labs, poked every 2 hours, multiple IVs and PICC lines. Then she had surgery, which lead to an epidural, catheter, more IV tubes, a feeding tube and a lot of pain. But it was all worth it when she was deemed CURED about a year later!
Nate
Sending out a BIG hello to all from sugar baby, Nate & I. Nate was born with Pierre Robins Sequence, but there always seemed to be something else lurking in the background that we couldn’t put our finger on. At 6 months old Nate suffered a convulsive seizure, as a result of extremely low blood sugar… And that was it. One minute I was making an early morning Sunday coffee and the next we found ourselves initiated into the world of hyperinsulinism (HI).
It’s been a steep learning curve, so far. Some days are FABULOUS. Other days the term ‘day’ itself seems too long a time frame, too far away to achieve, so we break it down into hours, sometimes minutes. Our lives are ruled by the clock, checking blood sugar levels, feeds & meds. Yet through all the ups and downs there is one thing that has remained constant and that is my beautiful little Nate. He is the same courageous, loving and happy little boy he was before HI, and his strength and cheeky character continue to blossom in spite of it.
No matter how unwell he is, you can guarantee Nate will be smiling, his wonderfully contagious smile, to everyone in his view. I couldn’t be prouder of my Sugar Baby and I’m honored to have been chosen to be his mum.

Julieta Joy
My sugar baby is Julieta Joy, she was born with an 18 blood sugar last summer. We were lucky enough that they checked her blood sugar as soon as she was born because she was unresponsive. She was diagnosed with hyperinsulinism when she was 5 days old, and she struggled in the NICU for about 3 months until we could stabilize her sugars and bring her home.
She currently eats high caloric formula through a g-tube every three hours and has to eat continuously overnight for 11 hours to maintain stable sugars. She also gets two injections twice a day. She is now 7 months old and is growing and meeting her milestones.
We hope that she did not have any brain damage due to her low blood sugars early on. She is the perfect baby, and transmits nothing but love to all around her. Her HI is non-genetic so we hope that she will someday outgrow this very difficult rare disease.

Jeremiah
This is Jeremiah. He is five years old and has no known mutation. He was diagnosed at 11 months old. Only on the 4th visit to the emergency room, after having is 4th seizure, was he diagnosed. When I brought him to the emergency room, after his second seizure, we were told he was just having night terrors. Then he was diagnosed with epilepsy, and finally with HI. His condition is managed with diazoxide and diet.
Aapo from Helsinki, Finland
Our son Aapo was born in February 2015 in Helsinki (Finland). 34 hours after birth his low blood sugar was noticed – he spent three weeks at the NICU in Helsinki and was diagnosed with hyperinsulinism. He has a mutation in the gene HNF4a1 and is diazoxide responsive – in September 2015 he was weaned off and is now cured! His gene mutation may cause diabetes later in his life. We are very grateful for all the great support we have received from the HI family during our journey and we hope our story will encourage other HI parents.
Ezra
Ezra was diagnosed with HI at the age of 5 months after a seizure. Although initially we thought he had focal disease, during surgery we discovered it was actually diffuse. He is currently being treated with octreotide injections during the day and overnight dextrose while he sleeps. He is a sweet and active 14 month old who is adored by his older siblings. We are so thankful he is a part of our family.

Kieran from Wisconsin
This is Kieran. He was diagnosed with CHI after a hypoglycemic seizure. He was hospitalized for two weeks at the Children’s Hospital of Wisconsin until he was diagnosed. He has a mutation in UCP2 and is responsive to diazoxide. He still struggles with low blood sugars and the affects of spending the first 12 months of his life with low sugar, but he is stubborn and determined not to let anything slow him down!

James and Matthew from New Jersey
We are from New Jersey and both our sons were born with transient hyperinsulinism. They were treated at the Children’s Hospital of Philadelphia (CHOP) where they both were put on a course of diazoxide and diruil. Both resolved after 5 months of treatment. Neither child carries the genes for HI, nor do my husband and I. I did not have gestational diabetes or hypothyroidism.
James, my oldest, was an emergency C-section and needed to be resuscitated at birth. The nurse who took care of him decided to check his sugar, so he was monitored since birth – we feel very lucky about that. Doctors at our local NICU could not figure out why his sugar wasn’t resolving so after a few weeks we were transferred to CHOP where he was diagnosed and treated for HI.
When I became pregnant with Matthew we were so worried he would have it too, but were assured he wouldn’t because there was no genetic cause. But, to be safe, we would check him when he was born. Unfortunately he was born with transient HI as well. CHOP’s first case of sibling transient hyperinsulinism. It was a rough start for both our boys but we are grateful that they recovered and are currently doing very well. Thank you for letting us share our story.

Leo
This is our 19 month old sugar baby, Leo. At 4 months old, he had a seizure and less than 3 days later, he was given the diagnosis of hyperinsulinism. We are very fortunate that he responds well to diazoxide and on “good” days doesn’t require more than 2 or 3 blood sugar checks. He has a mutation on the UPC2 gene, inherited from his father, who is non-HI. Apparently, there are less than 10 reported UPC2 gene mutations worldwide and the particular region of their mutation has never been reported before. We are traveling to CHOP in the very near future so Leo’s father can participate in a study as it relates to the UPC2 gene. We are excited for the opportunity to learn more and to contribute to the ongoing research regarding this very rare disease.
Leo is a happy, charming, silly little boy who takes his medicine like a champ and barely flinches during his blood sugar checks. He is a brave little guy who never ceases to amaze us each and every day. There have been some dark days in dealing with this disease, especially in the early days and it can be challenging when he’s not well or is being a picky toddler….but we feel truly blessed. We also feel incredibly grateful and blessed for the CHI Parents Forum; it is an incredible thing to be able to connect with other parents, worldwide, who can relate, understand and show support.

Ashlee
My name is Ashlee and I was diagnosed with HIHA when I was about 14 months old. I have always had to check my blood sugar many times each day, watch the amount of protein I eat and take a lot of medicine. It is really frustrating sometimes because I crave all of the foods that I should not eat.
My parents and I do a lot to advocate and help others with this disease. I have even tried new medicines in hopes of it helping manage my blood sugars. I think that living with this disease has helped me become really understanding and empathetic about people dealing with rare diseases.
I want to be a nurse and next year, when I am in 11th grade, I will be starting an early college program to start my nursing program prep. I told my mom that I dream of being a pediatric nurse for either CHOP or Cook Children’s Hospital and working in their hyperinsulinism clinics. They think that is a great goal for me to have!

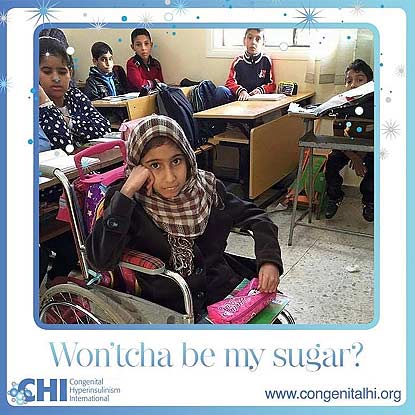
Fatima from Benghazi, Libya
This is beautiful Fatima. She lives in Benghazi, Libya where she lives with her loving family. Fatima is in a wheelchair because she cannot walk, the result of prolonged untreated hypoglycemia before she was diagnosed with hyperinsulinism hyperammonemia syndrome. Also, due to hypoglycemia, Fatima has trouble with her jaw and esophagus. Fatima wishes for a cure for hyperinsulinism hyperammonemia syndrome. Fatima loves to learn, reading and writing.
Asher from New Jersey
Hi everyone! This is my son Asher! We are from New Jersey! Asher was transported to the Children’s Hospital of Philadelphia where he was diagnosed with KATP defect with Diffuse Congenital Hyperinsulinism and Beckwith Wiedemann Syndrome, at only 2 days old! He had a near-total pancreatectomy (98%), appendectomy, and a fair share of tests done during my his month of life.
This has been quite an adventure for us. I cannot wait to see what the future holds for this little guy! He is already doing amazing things. He is one of the happiest babies that I know. I am very thankful for CHI, bringing all of these families together. Asher and I have made some wonderful friends! We wish all of the best to all of our fellow HI babies and families!

Harley from Australia
This is Harley from Australia. He was diagnosed with hyperinsulinsim at 4 months old. He is now 2.5 years old and not letting it slow him down. He is currently on diaxoxide to help keep him stable. Harley is always smiling and happy. He is a very determined little man who is always eager to explore and try new things
Paula from Catalonia
Paula is from Catalonia in Spain, near Barcelona. She has two mutations in the gene ABCC8. She has has taken diazoxide since she was two days old, although she has only a partial response to it.
We’ve had four years of very hard times, but we have also learned that the brightness in her eyes, is the biggest strength.
From her diagnosis, we have discovered many new words such as hyperinsulinism, dextrose infusion, diazoxide, ocreotide, pancreatectomy, gastrostomy, PET scan… although none of us wanted to discover them.
But we’re very thankful to the CHI family, it’s great to have friends that know exactly what you’re feeling, or what you’re worrying about, no matter where they live.

Marlee from Australia
“Hi, I’m Marlee and I’m from Australia! I’m 2.5yrs old and was diagnosed with hyperinsulinism at about a week old after giving Mum and Dad a huge fright as we were getting ready to head home from the hospital.”
“It’s been a rough ride since I was born but I am still one of the happiest, smiling kids you’ll meet.”
“I have to take a medicine called diazoxide to try and keep me stable and Mum or Dad checks my blood sugar levels anywhere from 3 times a day up to 10 or more on days where I’m not feeling the best and things become unpredictable.”
“The doctors don’t know really what the future brings for me and my hyperinsulinism so we just take each day as it comes and hope that things remain stable for now.”
“We are so grateful every day for all the support and love we get through CHI. Families from all around the world have made living with this condition much less isolating and just that little bit more bearable.”

Maxwell
Hi, I am Maxwell! I will be two years old in May, and I have hyperinsulinism/hyperammonemia (HIHA.) My blood sugars are managed by a high diazoxide dose and diet. I like to keep my family on their toes because my blood sugar drops when I’m teething and when I get sick, which has led to some extra hospitalizations. I have such a happy, easy going personality. I love keeping up with my big brother and snuggling my dog.
Penelope
Penelope was born with meconium aspiration that required ECMO treatment and during recovery we discovered she had ‘blood sugar issues,’ that turned out to be congenital hyperinsulinism (HI). She responded well to diazoxide and it later transpired after further testing that her HI was the result of Beckwith Weidemann syndrome. It is particularly difficult for babies with both as it is quite a small cross section and can be overwhelming dealing with not one, but two rare diseases! Penelope is currently being trialed off diazoxide and is doing great so far!

Olivia from Texas
I found out something was going to be wrong with Olivia two weeks before I had her, but nobody knew what. On December 18th, 2013 Olivia was born with a blood sugar of 4. Since then I have literally felt my heart break, but at the same since, my heart has never felt so much joy.
In 2 years, Olivia has stopped breathing on me more times than any parent should have to experience. I have seen the worst. Olivia had 98% of her pancreas removed in January 2015. After her surgery, Olivia had problems with pain and keeping her airway open. I spent a lot of days in the PICU in Texas. I knew this is what rock bottom felt like. On our 3rd day in the PICU the nurses started shutting the curtains all around us, but ours had a little sliver still open, and I saw that another little one did not made it (for different reasons), yet I was still holding Olivia, and she was fighting. I knew from that day, I need to keep fighting for this little lady, because she has hit rock bottom, and has kept fighting. Olivia has two rare diseases hyperinslinism, and Kabuki, neither one of which, I would wish upon someone. Olivia still suffers from HI even after the surgery. Olivia still take meds for low blood sugar, she still needs her blood sugars checked throughout the day. Olivia has to eat every 3 hours, and still needs to be on continuous dextrose at night.

When Olivia was born all I wanted was some answers: was she going to walk? Would she ever eat on her own? Would she be able to talk? Nobody was ever able to answer these questions. I was told “take it day by day, and celebrate each milestone she hits.”
Now Olivia is almost 26 months old, she is walking, she is eating on her own, and she is trying to form words.
Hyperinsulinism has changed my life, I have lost a lot in 26 months, but I have gained so much more. I see the world differently, people differently. I understand the saying, “It takes a village to raise a child.”
Alyssa
Alyssa is our 9 year old sugar baby! She was diagnosed at 10 months old and has been on the medication, diazoxide, since then. Alyssa was named 2015 Salem County Children’s Miracle Network Ambassador. She has ridden in a few parades raising awareness for congenital hyperinsulinism. Alyssa is such a brave, strong little girl and she lights up our life with her beautiful smile!

Evelyn
This is my sugar baby Evelyn. She spent the first few weeks of her life dealing with low blood sugars in the NICU, which led to her diagnosis of hyperinsulinism. Evelyn also had aspiration issues which led to another harrowing hospitalization where we learned she could not swallow thin liquids. An NG tube was placed, and she was put on oxygen in order for her lungs to heal. The issues continued to add up, which led the team of doctors to suggest genetic testing. We wouldn’t learn of her mosaic Turner syndrome until she was 4 months old. At the time of her diagnosis, her geneticist could only find one other documented case of hyperinsulinism and mosaic turner syndrome. The continued feeding difficulties, and overnight feeds needed for blood sugar management led to a g-tube being placed at 4 months old.
Evelyn is managing her HI well on diazoxide and g-tube feeds. Despite all of her difficulties, she is alive and thriving. She is a happy, smart, energetic, loving 3 year old.

Annika June
“Hi, I am Annika June! I was diagnosed with congenital hyperinsulinism (HI) diffuse disease at two and a half months old. After being transferred from our hospital in NY to CHOP, I had a 50% pancreatectomy and g-tube placed.”
“Now, that I am two years old, I keep my blood sugar levels up with frequent meals and snacks during the day and continuous dextrose through my ‘tubie’ overnight. My favorite things to do are playing with my big brother and blowing bubbles!”

Gracie from Lubbock, Texas
This is Gracie from Lubbock TX. She is now 6 years old and still dealing with developmental delays and challenges. She was diagnosed at 4 months old. Her symptoms appeared hours after birth but the nursery mistook it for transitional diabetes and sent us home … my only wish is for hospitals to stop discharging any infant showing any kind of signs of hypoglycemia, even if it could only be transitional diabetes … keeping her longer in the hospital could have meant a chance at a normal life … comparing Gracie’s development to her younger sister’s shows how much of a deficit Grace has … early diagnosis could mean less brain damage, and seizure history or epilepsy would be less likely … ALL BABIES DESERVE THAT MUCH!

Ava
This is my sugar baby..Ava had a rough start in life but she is now nearly 7 years old and managed solely by diet and her pump at night. We are so proud of the way Ava handles her condition every day.She is amazing and we love her very much!

Joslyn
Joslyn Gabriella is our one and only sugar baby! Lately it’s been a struggle keeping her blood sugar levels up. But now it’s looking better and her doctor is even considering lowering her dose of diazoxide. Joslyn is one very strong and determined little girl and we pray every day that she’ll outgrow her hyperinsulinism.

Juliana
I am Juliana Elizabeth, 20 months! I am still on this HI journey and my low sugar continues to be managed with Diazoxide. I continue to have my sugars checked daily and follow-ups at CHOP. I also have a few other medical issues that I am told don’t all relate to my HI … doctors say I am one of a kind … my parents say I am their perfect little girl! Most people think I am 2-3 years old between my long hair and how tall I am, but I am still only a year old! I like to do puzzles, color, run around and play with my older brother, Justin. I also LOVE “coco” (what I call chocolate), but that’s okay if I eat sweets because I am a Sugar Baby.
It is important to continue to spread awareness of HI, the rare disease I and others have, as well to educate people to prevent the serious side effects it can cause if not properly diagnosed early on and treated.

Kinley
Kinley – my little sugar baby! It is believed that her hyperinsulinism is resolving, and she is thankfully now medicine free. However, lately it seems that maintaining her blood sugar at a safe level is a daily struggle. She is such a strong, beautiful and resilient little girl.




